Dental Labs, Dentist
Occlusion and caries: Ongoing zirconia challenges
Zirconia crowns are well known as the most-used ceramic restoration in dentistry. Dr. Gordon Christensen provides some potential solutions for a few of their most important challenges.
Gordon J. Christensen, DDS, PhD, MSD
“I have been practicing for many years, and most of the indirect restorations I have placed in the past could be cemented with correct occlusion as they came from the laboratory. However, in recent years, I am seeing some crowns that are not even close to touching the opposing arch of teeth, and others are too high. These crowns come from my usual laboratory that has had near-optimal occlusion on the crowns in the past. Additionally, I still have some zirconia crowns coming off in service. What can I do about these challenges?”
Dr. Christensen: Both you and I are seeing the same problems, and I have several potential reasons and solutions to share.
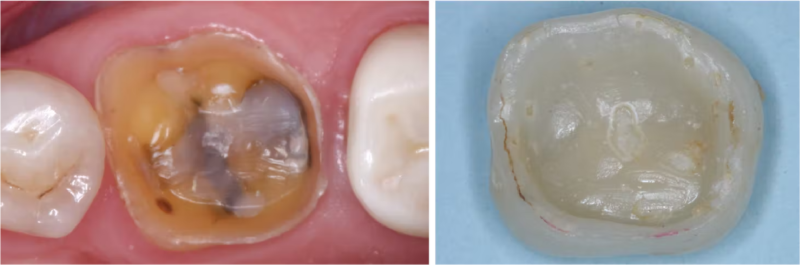
Labs are making crowns out of contact with the opposing arch (figure 1). Some labs are making crowns up to 0.5 mm too low (500 microns or the thickness of at least 10 human hairs) as measured by Clinicians Report (CR) scientists. This reduction in crown height reduces the completed restoration occlusal thickness, potentially compromising crown strength and causing tooth extrusion of both the tooth being crowned and the opposing tooth, as well as stress on adjacent teeth.
Figure 1: Note the significant lack of occlusal contact on this zirconia crown example as sent from a large dental laboratory.
Why would technicians do this? Currently, the most popular crown types—zirconia and lithium disilicate—are very difficult to reduce in height and difficult to finish and polish smooth in the mouth, taking clinical time and frustrating the dentist and patient. The technician and the dentist would like to have the patient say the crown feels just right when closing the two arches together. Making the crown shorter with no occlusal contact avoids removal of ceramic on the occlusal/incisal surface when seating.
Most zirconia and lithium disilicate crowns are initially one color without significant translucence. Thus, most ceramic crowns have a layer of low-fusing ceramic fired over them to provide individual characterization of color and translucence on the crown. If the occlusal/incisal crown surface is adjusted, removing the superficial layer of low-fusing ceramic, the underlying zirconia or lithium disilicate is exposed and the restoration’s color and translucence are compromised.
In discussions with CR scientists and clinicians, they disagree with placement of superficial low-fusing ceramic. They have proven that the superficial glaze and stain wear off over time and wear the opposing teeth until worn off (personal communication, Rella Christensen, PhD).
Successful cementing of zirconia crowns: Still a problem
Zirconia crowns in dentistry: Uses, clinical challenges, and solutions
Some labs are spacing the intaglio (internal) surfaces of crowns to reduce seating difficulty as measured by the CR science team (figure 2). You have probably noticed that many current zirconia crowns do not have a definitive seating location and tend to be mobile on the tooth until cemented. This unfortunate situation is directly related to internal spacing. So, how much internal spacing is necessary for optimum seating?
I strongly suggest dentists should communicate with their lab technicians to minimize the external and internal spacing of zirconia crowns.
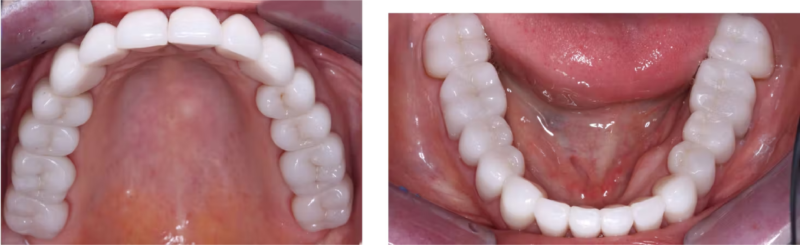
Open margins are a problem. When the crown internal is spaced digitally, the margin is also spaced. Are dentists using cariostatic cement to fill those open margins? Thankfully, most dentists (from CR survey data) are using resin-modified glass ionomer (RMGI). Popular and proven examples are 3M RelyX Luting Plus and GC FujiCEM Evolve, which release significant fluoride for potential reduction of future caries involvement on the margins. However, many dentists are using resin cements for zirconia crown cementation, which have at least 2% polymerization shrinkage, resultant microscopically open margins, and no cariostatic properties.
Assuming you have followed the narrative above, most zirconia crowns cemented with the resin cement technique are essentially a strong zirconia roof on a potentially cariogenic composite resin cement. Logic says future marginal caries will be present on zirconia crowns cemented with resin cement (figure 3).
Use resin-modified resin cement until additional long-term research is completed on my suggestion below.
Figure 3: Open margin on a crown with caries that almost exposed the pulp when removed was seated with resin cement.
A possible solution for the cement challenge with zirconia crowns. In the 1970s and 1980s, conventional glass ionomer (GI) cements were used routinely. Later, about 20% resin was added to modifications of these cements, resulting in RMGI cements as discussed above.
Why aren’t conventional GI cements popular in North America? Infrequently and without any supported research reason, significant postoperative tooth sensitivity was observed, which led most dentists to choose other cements. Can that be overcome today? Yes!
Clinicians Report Foundation scientists have accomplished long-term research on glutaraldehyde-containing materials such as Zest Dental Solutions MicroPrime G, Kulzer Gluma, and several others. This data has been published in Clinicians Report.1 These liquids contain 5% glutaraldehyde and 35% HEMA. When applied to tooth preparations for two one-minute applications just before cementing a crown, they coagulate the tooth collagen, closing the dentinal tubules and effectively eliminating postoperative tooth sensitivity. Another major reason for their use is that the application technique also effectively disinfects the tooth preparation.
Proven conventional GI cements are available. Two well-known brands are 3M Ketac Cem and GC Fuji I. Such cements do not have the undesirable polymerization shrinkage of resin or the slightly less shrinkage of resin-modified cements. They have natural chemical chelation (bonding) to tooth structure, and they have proven preventive properties related to fluoride release.
Here’s a personal empirical observation from my long-term practice experience. Remember Dr. David Sackett’s classic statement about evidence-based medicine (EBM)? He is the person often credited with initiating and supporting evidence-based practice. This is a direct quote from Dr. Sackett: “EBM is the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients. The practice of EBM means integrating individual clinical experience with the best available clinical evidence from systematic research.”2
Editor’s note: This article appeared in the February 2023 print edition of Dental Economics magazine. Dentists in North America are eligible for a complimentary print subscription. Sign up here.
References
- How to predictably reduce post-op tooth sensitivity and caries. Clinicians Report. 2020;13(10).
- Sackett DL, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312(7023):71-72. doi:10.1136/bmj.312.7023.71
Author’s note: The following educational materials from Practical Clinical Courses offer further resources on this topic.
One-hour videos:
- Strong, Comfortable, Esthetic Rehabilitations with Zirconia (Item #V1942)
- Cementing Restorations—Proven and Successful (Item #V1921)
Three-hour virtual course:
- Christensen’s Most Frequent Failures and How to Avoid Them (Item #X4740)
- Making Occlusion Work for Your Practice (Item #X3515)
For more information, visit our website at pccdental.com or contact Practical Clinical Courses at (800) 223-6569.